HESA Committee Report
If you have any questions or comments regarding the accessibility of this publication, please contact us at accessible@parl.gc.ca.
THE HEALTH OF LGBTQIA2 COMMUNITIES IN CANADA
Introduction
On 16 April 2018, the House of Commons Standing Committee on Health agreed to “undertake a study on LGBTQ2 health in Canada in order to develop recommendations on actions that the federal government can take, in partnership with the provinces and territories.”[1] The Committee held seven meetings on this topic between 28 February and 9 May 2019, hearing from 33 witnesses and receiving 44 briefs. As part of the study, the Committee travelled to Montreal, Winnipeg, Calgary and Vancouver to meet with six organizations in April 2019. The witnesses that the Committee heard from and the groups that it met with included community organizations that provide services to lesbian, gay, bisexual, trans, queer, intersex, asexual and two-spirit (LGBTQIA2) communities, community-based research organizations, academic researchers, provincial agencies and volunteer groups that provide peer support.
This report examines the main health challenges facing LGBTQIA2 communities in Canada and identifies ways in which the federal government, in co‑operation with the provinces and territories, can address the health inequities that these population face. First, the report sets out the definitions and terminology used to refer to LGBTQIA2 persons. The second section of the report outlines the mental, physical and sexual health status of LGBTQIA2 communities in Canada based on available data. Next, the report examines factors that contribute to health inequities among gender and sexual minorities, as well as the way identity factors and certain determinants of health intersect and affect the health of LGBTQIA2 communities. The report concludes by presenting potential solutions and a series of recommendations to the federal government for improving the health of Canada’s LGBTQIA2 communities.
DEFINITIONS AND TERMINOLOGY
Gender and Sexual Minorities
A number of terms and abbreviations are used to describe individuals whose gender identity or sexual orientation is different from that of the majority of people.[2] This report will use the abbreviation LGBTQIA2 (lesbian, gay, bisexual, trans, queer, intersex, asexual and two-spirit).[3] The terms “gender and sexual minorities” and “gender and sexual diversity” will also be used to refer to individuals who identify as a different sexual orientation or gender identity from the general population.
The witnesses explained to the Committee that LGBTQIA2 communities are diverse and heterogeneous. This abbreviation includes terms relating to sexual orientation—for example, identifying as lesbian, gay or bisexual—and terms specifying gender identity—for example, identifying as trans. LGBTQIA2 individuals may therefore identify as a different sexual orientation or a different gender identity from most of the population, or both, as Joël Xavier, Administrator at the Conseil québécois LGBT, pointed out during his appearance before the Committee:
I am a gay man and a trans individual. Yes, we can in fact represent two letters of the acronym.[4]
With regards to sexual orientation, Lori Ross, Associate Professor at the University of Toronto, informed the Committee that this characteristic relates to both behaviour and sexual attraction. Some individuals who do not identify as LGBTQIA2 may have sexual relations with people of the same sex (sexual behaviour) or be sexually attracted to people of the same sex.[5]
Regarding gender identity, Alex Abramovich, Independent Scientist at the Centre for Addiction and Mental Health, explained that people who identify as the sex they were assigned at birth are referred to as “cisgender.”[6] The term “trans” indicates people who do not identify as the sex they were assigned at birth. Jack Woodman, President of the Canadian Professional Association for Transgender Health, added that the term “trans” can include transgender or non-binary individuals.[7] Quinn Bennett of Trans Care BC noted that not all trans persons want or need medical interventions to live comfortably in their gender.[8]
As for intersex persons, the Committee received briefs stating that up to 1.7% of the population is born with intersex variations affecting the gonads or other sexual organs, chromosomes or hormones.[9]
Witnesses also explained to the Committee the meaning of “two-spirit.” Albert McLeod of Two-Spirited People of Manitoba said that the term was created in the 1990s to describe Indigenous people who adopt roles, attributes, dress or attitudes with various gender identities for personal, spiritual, cultural or social reasons.[10] The concept therefore encompasses the ideas of sexuality, gender and spirituality.[11] Other witnesses emphasized that “two-spirit” can have different connotations depending on the person, and individuals are encouraged to carry out research on the way gender and sexual diversity was expressed in their Indigenous cultures before colonization.[12]
Size of the LGBTQIA2 Population in Canada
Witnesses informed the Committee that determining the exact number of people who make up gender and sexual minorities in Canada is difficult. The results of Statistics Canada’s Canadian Community Health Survey (CCHS) for 2015–2016 indicate that 1.4% of Canada’s population aged 15 and older identify as homosexual and 1.5% identify as bisexual.[13] In addition, Rainbow Health Ontario estimates that approximately 7.3% of Ontarians identify as lesbian, gay or bisexual and that about 0.6% identify as trans.[14] These estimates exclude people who engage in homosexual behaviours but do not identify as being part of a sexual minority.[15] Finally, Trans Care BC estimates that between 1% and 3% of the population are trans, but that only 0.3% to 0.6% of the population could need gender affirming medical interventions.[16]
The Committee learned that estimating the number of trans people in Canada is difficult because Statistics Canada surveys have not yet asked questions about gender identity.[17] In a brief submitted for the study, Statistics Canada stated that it plans to fill this gap. Questions on sex at birth and gender identity that will enable Canadians to report their identity in a non‑binary fashion are currently being tested for inclusion in the 2021 Census.[18]
THE HEALTH OF LGBTQIA2 PEOPLE
“Strong mental health supports good physical, sexual and social health…. [S]exual health is only one of several components of health and wellness. Physical, social and mental health needs are often drivers for more healthy … sexual behaviours.”[19]
Greg Oudman, Executive Director, Health Initiative for Men
Mental Health
During the study, the Committee learned that the mental health status of the Canadian population varies with sexual orientation and gender identity.
Figure 1—Fair or Poor Perceived Mental Health, By Sexual Orientation
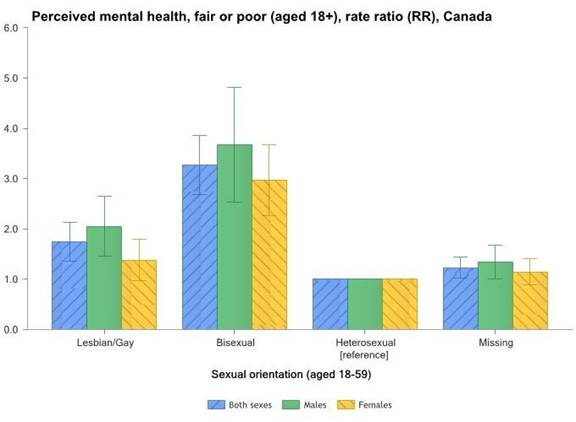
Source: Pan-Canadian Health Inequalities Data Tool, 2017 Edition.
Figure 1 shows CCHS data on Canadians whose perceived mental health is fair or poor, broken down by sexual orientation. The data reveal that bisexual and homosexual individuals are two to four times more likely than heterosexual individuals to perceive their mental health as fair or poor. In addition, bisexual people are more likely than homosexual people to perceive their mental health as fair or poor.
A number of witnesses told the Committee that lesbian, gay and bisexual people are more likely than heterosexual people to report having mood or anxiety disorders.[20] Moreover, bisexual individuals are at greater risk of suffering from a mental health disorder during their lifetime than gay or lesbian individuals.[21]
Lori Ross, University of Toronto, reported that gay and lesbian people are three and a half to four times more likely to report having suicidal thoughts during their lifetime than heterosexuals. Ms. Ross also informed the Committee that a recent survey of 400 bisexual youth in Ontario found that 30% of them reported having suicidal thoughts over the past 12 months.[22]
The Committee heard that the mental health status of Canadian youth and adults also varies with their gender identity. The Trans PULSE study, conducted in 2009 and 2010, found that 60% of trans people reported having depression; 36% said they had suicidal thoughts in the past 12 months and 10% indicated that they had attempted suicide. Among trans youth, up to 65% reported having suicidal thoughts in the prior 12 months.[23]
Multiple witnesses and organizations that submitted briefs highlighted the negative effects of “conversion therapy” on the mental health of LGBTQIA2 people.[24] This term may be defined differently by stakeholders. Nova Scotia defines “change efforts” as “any counselling, behaviour modification techniques, administration or prescription of medication or any other purported treatment, service of tactic used with the objective of changing a person’s sexual orientation or gender identity.”[25] Ontario refers to treatments or services that “seek to change the sexual orientation or gender identity of a person.”[26] The Committee also heard that “conversion therapy is an umbrella term for practices that intend to change an individual’s sexual orientation and gender identity.”[27]
There is evidence that 4% of men who identify as being in a sexual minority report having undergone conversion therapy.[28] Conversion therapy appears to produce feelings of shame, low self-esteem, depression, anxiety and substance abuse.[29] Travis Salway, Post-doctoral Research Fellow at the University of British Columbia, explained to the Committee that his research indicates that one-third of men who have undergone conversion therapy have attempted suicide.[30]
A number of witnesses and organizations submitted briefs recommending to the Committee that conversion therapy should be banned in Canada under the Criminal Code.[31]
Physical Health
Few data are available on the physical health of LGBTQIA2 people in Canada. Lori Ross, University of Toronto, noted that “we’re only beginning to understand those kinds of differences [regarding physical health], because we’ve only started to ask those questions.”[32] Still, the witnesses pointed to two aspects of the physical health of LGBTQIA2 individuals for which data exist and reveal inequities: chronic diseases and cancer.
Chronic Diseases
The results of the CCHS reveal that the prevalence of asthma is 16% among lesbian and bisexual women, compared with 9% among heterosexual women.[33] Figure 2 shows the rate of arthritis broken down by sexual orientation. Bisexual and lesbian individuals are more likely to suffer from arthritis than their heterosexual counterparts.
Figure 2—Rate of Arthritis in Canada, By Sexual Orientation
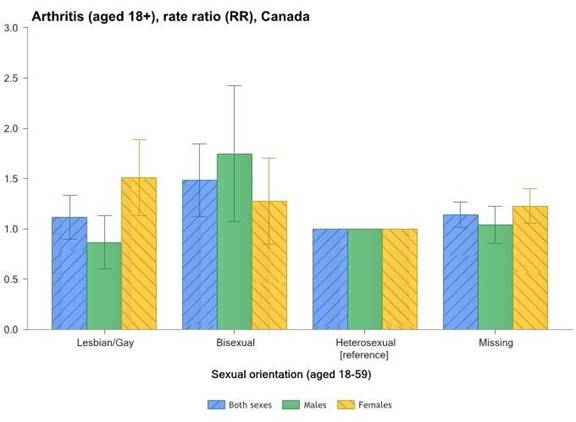
Source: Pan-Canadian Health Inequalities Data Tool, 2017 Edition.
Rainbow Health Ontario informed the Committee that the limited data that are available show a greater prevalence of cardiovascular diseases, some types of cancer and respiratory diseases among LGBTQIA2 Canadians compared with heterosexual Canadians. Chronic diseases also tend to appear earlier among LGBTQIA2 individuals.[34]
Cancer
Some cancers are more common among LGBTQIA2 individuals. Appearing before the Committee, Dr. Tinus Wasserfall, Family Doctor at Spectrum Health, said that gay, bisexual and other men who have sex with men (gbMSM) have an anal cancer rate of 45 per 100,000 compared with 1.5 to 2 per 100,000 for the general population. Human papillomavirus (HPV) infection is a very common infection and is present in 90% of anal cancers.[35] As a result, Dr. Wasserfall recommended that gbMSM undergo screening exams for anal cancer and be vaccinated for HPV no matter their age.[36]
Sexual Health
Sexually Transmitted and Blood-Borne Infections
Gender and sexual minority individuals are at greater risk of contracting a sexually transmitted and blood-borne infection (STBBI) such as syphilis and human immunodeficiency virus (HIV).[37]
The Committee learned that gbMSM are overrepresented among HIV cases and at much greater risk of being infected by HIV than anyone else in Canada.
“I’ll never know for certain if I would be HIV-positive if I weren’t gay, but I do know that as a gay man, I was 131 times more likely to be infected than my straight counterparts were.”[38]
Brook Biggin, Founder, Edmondon Men’s Health Collective
In 2016, gbMSM accounted for 48% of new HIV cases in Canada, despite making up just 3% to 5% of the adult male population.[39] In addition, Dr. David Moore, Research Scientist, Epidemiology and Population Health Program, British Columbia Centre for Excellence in HIV/AIDS, noted that, despite scientific progress, the number of new diagnoses among gbMSM in Canada each year has held steady for 10 years. Dr. Moore reported that “HIV remains a fundamental threat to the health of gbMSM and results in significant costs to the Canadian health care system.”[40]
The Committee was told that a number of actions are needed to address the high rates of STBBIs among LGBTQIA2 individuals, particularly gbMSM. First, Dr. Mark Gilbert pointed out that the federal government published A Pan-Canadian Sexually Transmitted and Blood-Borne Infections Framework for Action in 2018 that recognizes the impact that these infections have on trans individuals and gbMSM in Canada. However, he recommended that the Canadian Guidelines on Sexually Transmitted Infections and national resources on sexual health be updated to reflect all gender identities.[41]
Second, the Committee discovered that Canada has fallen behind other countries with regards to access to new testing technologies for STBBIs. There are no licensed home or self-testing kits for STBBIs in Canada, even though these tests have proven effective in other countries. Dr. Mark Gilbert recommended that the federal government accelerate its licensing of testing kits and encourage the companies that make them to market them in Canada.[42]
At a meeting with the organization Head and Hands in Montreal, the Committee learned that some queer women have trouble getting tested for STBBIs because some health care providers do not believe these women engage in “genuine sexual relations.” [Translation][43]
To eliminate the threat that HIV poses to the health of gbMSM, as well as the Canadian population as whole, the Committee heard that not only is it necessary to improve access to new testing technologies but also to HIV treatment. Dr. David Moore explained that access to modern antiretroviral treatment has been highly effective in preventing the development of HIV/AIDS and prevention of premature death among people living with HIV/AIDS.[44] In addition, he explained that more recent research has found that effective HIV treatment is 100% effective in preventing HIV transmission, which is referred to as treatment as prevention (“TasP”).[45]
Despite this success rate, the Committee heard that not all provinces and territories in Canada offer full coverage of the costs of antiretroviral treatment. Currently, all five federal prescription drug coverage programs[46] and six provinces and territories, including British Columbia, Alberta, New Brunswick, Prince Edward Island, Northwest Territories and Nunavut, offer public coverage of HIV medications without out-of-pocket costs.[47] The remaining jurisdictions provide coverage for these medications but with varying forms of out-of-pocket payments, including co-payments, deductibles and premiums through their various public drug coverage programs.[48] Most of these out-of-pocket payments are waived for Canadians with low incomes or those living on social assistance.[49] Gerry Croteau, Executive Director, Gilbert Centre for Social and Support Services explained that the cost of HIV medications can exceed $1,000 per month, which can lead to significant out-of-pocket costs for individuals who do not have access to private drug coverage, or have limited coverage through public plans.[50] In a written follow-up submission to the Committee, Gary Lacasse, Executive Director, Canadian AIDS Society explained that of the 52,220 individuals who have been diagnosed with HIV in Canada, 39,790 are currently receiving treatment for the disease.[51] Consequently, witnesses recommended that the federal government support access to HIV medications free of charge for all Canadians.[52]
Dr. Moore also explained to the Committee that more recently research has shown that Truvada, a drug which is a combination of two antiretroviral medications and is known as “PrEP”), is nearly 90% effective in preventing HIV acquisition among gbMSM who are at high risk for infection.[53] The Committee heard that British Columbia’s Centre for Excellence in HIV/AIDS has offered the drug free of charge to individuals at high risk of acquiring HIV since January 2018. As a result, the province is experiencing the lowest rates of new HIV diagnosis since the mid-1990s. Despite this progress, Dr. Moore explained that not all provinces and territories provide coverage for PrEP as part of their public drug coverage plans (see Table 1) and where public drug coverage is provided, individuals may also face out-of-pocket costs as they do with other HIV medications, as noted above. He therefore similarly recommended that the federal government provide free access to PrEP for individuals at risk of HIV infection. Finally, he explained that there is also a need to raise awareness of the availability of PrEP to promote its uptake among gbMSM.[54]
Table 1—Federal, Provincial and Territorial Prescription Drug Coverage of Pre‑exposure prophylaxis (PrEP)
Jurisdiction |
Coverage of Pre-exposure Prophylaxis (PrEP) |
Alberta |
Yes |
British Columbia |
Yes |
Manitoba |
No |
New Brunswick |
Yes |
Newfoundland and Labrador |
Yes |
Northwest Territories |
Yes |
Nova Scotia |
Yes |
Nunavut |
Yes |
Ontario |
Yes |
Prince Edward Island |
No |
Quebec |
Yes |
Saskatchewan |
Yes |
Yukon |
No |
Federal Non-Insured Health Benefits Program |
Yes |
Source: Adapted from Toronto General Hospital Immunodeficiency Clinic, ”Provincial and Territorial Coverage of ARV drugs for HIV prevention across Canada: Post-exposure prophylaxis (PEP) and Pre-exposure prophylaxis (PrEP)” December 2018.
Use of Alcohol, Tobacco and Other Substances
The Committee heard that the prevalence of alcohol abuse, smoking and certain drug use is higher among LGBTQIA2 people than heterosexual people. This behaviour affects the physical, mental and sexual health of these communities.
Lesbian and bisexual women are 1.64 times more likely to use alcohol heavily than heterosexual women.[55] The smoking rate among the various LGBTQIA2 communities ranges from 24% to 45% and is highest among bisexual individuals.[56] By comparison, just 16% of the general population smoked in 2012.[57] One of the goals of Canada’s Tobacco Strategy is to target certain groups, including LGBTQIA2 people, in order to reduce smoking in Canada.[58]
It appears that gbMSM are also more likely than heterosexual men to use drugs. The Committee heard that drug use in this community may occurs in the context of sexual relations with a partner.[59] When the Committee met with REZO on its premises in Montreal, the organization reported that gbMSM who need services to address drug addiction in the context of sexual relations have trouble obtaining suitable services. REZO explained that addiction service providers have difficulty understanding that sexuality is central to their addiction.[60]
Heavy alcohol and tobacco consumption increases the risk of developing diseases such as cardiovascular disease, cancers, and respiratory, kidney and liver diseases. These risks are even greater for people with HIV.[61]
The Committee also learned that, for some members of gender and sexual minorities, mental health disorders coincide with increased use of substances such as tobacco, alcohol and other drugs, and this combination can lead people to adopt riskier sexual behaviours.[62]
Availability of Data on The Health of LGBTQIA2 Communities in Canada
The Committee heard that the data used to measure health among Canada’s LGBTQIA2 communities are mainly gathered by Statistics Canada’s annual CCHS survey, which has included a question on sexual orientation since 2003. Some data on the health of LGBTQIA2 communities comes from community-based participatory research conducted by various organizations and researchers in Canada.[63]
As of this year, the CCHS includes questions on sex at birth and gender identity and a modified question on sexual orientation. These last two questions allow respondents to provide a personalized answer in order to collect more varied information on sexual orientation and gender identity.[64]
Statistics Canada also informed the Committee that the 2019 edition of the Canadian Health Survey on Children and Youth (CHSCY) includes questions on sex at birth, the child’s gender identity and sexual attraction.[65]
However, witnesses noted that the data generated by the CCHS are limited because the question on sexual orientation is only asked of respondents aged 18 to 59, which restricts the amount of data available on the health of older LGBTQIA2 adults and LGBTQIA2 youth.[66] While the question on sexual orientation will allow for a write-in response starting in 2019, it does not take into account other dimensions of sexual orientation such as sexual behaviour and sexual attraction.[67]
The Committee also learned that health problems are less well documented among some LGBTQIA2 communities than others. Fewer data on the health of lesbian, bisexual and trans individuals are available than for gbMSM.[68]
Finally, the sample sizes of people who are members of gender and sexual minorities in Statistics Canada surveys do not allow for intersectional analyses to understand the health of Indigenous or racialized gender and sexual minorities.[69]
FACTORS CONTRIBUTING TO HEALTH INEQUITIES IN LGBTQIA2 COMMUNITIES
The Committee heard that a number of factors contribute to the physical, mental and sexual health inequities experienced by Canada’s LGBTQIA2 communities. These factors may be social, legal or identity-related (age or ethnocultural background) or linked to determinants of health such as access to health care. This section examines the factors witnesses highlighted as contributors to health inequities for gender and sexual minorities.
Social Factors
The health inequities experienced by LGBTQIA2 individuals in Canada are partly due to the stigmatization of gender and sexual minorities and the discrimination they can face in Canadian society. LGBTQIA2 people are stigmatized in part because homosexuality was long considered an illness.[70]
Gabriel Girard, Researcher at the Centre de recherche de Montréal sur les inégalités sociales, explained that the heteronormative and cisnormative nature of Canadian society—the fact that its practices and conventions are based on people being heterosexual and cisgender—contributes to LGBTQIA2 people feeling shame about their sexual orientation or gender identity.[71]
A number of witnesses described the discrimination that trans, non-binary and bisexual individuals endure. Canadian society also seems to render gender and sexual minority women invisible.[72]
Minority Stress
The discrimination and stigmatization that gender and sexual minorities experience can be internalized and contribute to “minority stress.”[73] Travis Salway, Post-doctoral Research Fellow at the University of British Columbia, explained this issue to the Committee:
Everyone experiences daily stressors—a late bus, a deadline at work. Sexual minority people, however, experience additional stress because of their minority status.… The stigma lodges itself [inside us] and slowly kills us from the inside.[74]
The Committee learned that minority stress takes numerous forms and accumulates over time through repeated exposure.[75] For example, LGBTQIA2 individuals may have to “come out of the closet” on multiple occasions, or sometimes every day.[76] Their sexual orientation or gender identity may be revealed against their will.[77] They also need to assess their situation to see if it is safe to disclose their sexual orientation or gender identity, and this decision is particularly stressful.[78]
For me, I come out every day at work…. I take appointments to fix people’s devices. Once a day there’s someone who asks me if I have a girlfriend or kids. I come out unabashedly to them to prove the point that there’s really no reason to assume that nowadays.[79]
Washington Silk of KW Counselling Services told the Committee that minority stress is directly linked to psychological distress and higher suicide risk among LGBTQIA2 communities.[80] Lori Ross of the University of Toronto pointed out that the accumulation of stress may also contribute to earlier onset of certain chronic diseases among LGBTQIA2 people.[81]
Legal Factors
The witnesses recognized that, while many advances in LGBTQIA2 rights have been made in recent decades, this progress has not gone far enough.
In Canada…, LGBTQ+ individuals have practically obtained equal consideration before the law…. However, legal equality is not true equality. In other words, recognition of same sex couples and implementation of anti-homophobia policies are indisputable achievements, but they are often offside with the experience of many LGBTQ+ individuals.[82]
Moreover, as Bill Ryan of McGill University pointed out, “The slow movement towards equality is lived asymmetrically depending on what initial in the acronym LGBTQIA2 one identifies with.”[83]
The Committee learned that the Criminal Code can—in criminalizing a person’s failure to disclose their HIV-positive status or permitting certain surgeries on intersex people—contribute to the stigmatization of LGBTQIA2 communities.
The witnesses explained how the criminalization of HIV non-disclosure stigmatizes people living with HIV and gbMSM, who are overrepresented in that group.[84] The Criminal Code does not contain any provisions that specifically address HIV non-disclosure.[85] However, the Supreme Court of Canada ruled that HIV non-disclosure in certain circumstances where there is a “realistic possibility of transmission” could invalidate consent to sexual activity, which could lead to charges of aggravated sexual assault (section 273) and aggravated assault (section 268).[86]
On 1 December 2018, the federal government announced a new directive concerning prosecutions of HIV non-disclosure cases. The new directive recognizes that over-criminalization of HIV non-disclosure discourages many people from being tested and seeking treatment. The directive sets out the specific situations in which prosecutions should not occur.[87]
The Committee notes that the House of Commons Standing Committee on Justice and Human Rights undertook a detailed study on the criminalization of non-disclosure of HIV status in the spring of 2019. It is expected that a report on this study will be tabled to the House of Commons.[88]
Richard Matern of Egale Canada informed the Committee that section 268 of the Criminal Code allows surgeries on intersex infants and children with the consent of their parents or guardians, but without the consent of the infant or child, a practice that can stigmatize intersex people.[89]
Furthermore, some witnesses told the Committee that restrictions on blood donations by gbMSM are a factor in their stigmatization.[90]
Intersectionality
The image that often comes to mind when we think about LGBT communities is of young, white, fit gay men at pride events. However, our communities are very diverse. People live in big cities, small towns, on and off reserves and up north. Our communities include small children through to people in their nineties and beyond. We’re from all cultures, ethnicities, races and faiths. Our communities include francophones, people with a broad range of mother tongues, and newcomers, including refugees. Our communities also include people who are homeless, poor, middle income, and high income.[91]
A number of witnesses emphasized that the heterogeneous make-up of LGBTQIA2 communities calls for intersectional analysis in order to understand the health inequities they face.[92] The health of the members of these communities is influenced by sexual orientation and gender identity, but also by other identity factors and determinants of health.[93]
Gabriel Girard explained intersectionality as follows: “Intersectionality is really a … guide to help us pinpoint the main areas of vulnerability.”[94] The evidence revealed that some intersections create more serious problems than others.[95] The witnesses suggested to the Committee that health policies and programs should focus on certain intersections.
The Committee learned that Health Canada and the Public Health Agency of Canada use sex and gender-based analysis plus (SGBA+) in developing, programs, policies and research activities. Using SGBA+ and taking into account other identity factors such as sexual orientation enables the government to take coordinated action to reduce the health inequities facing the LGBTQIA2 communities.[96]
Housing
The Committee heard that LGBTQIA2 youth are at greater risk of being homeless than heterosexual and cisgender youth. This disparity affects their health and well-being. Witnesses estimated that, of the 40,000 homeless youth in Canada, between 25% and 40% identify as LGBTQIA2.[97] Family conflict relating to sexual orientation or gender identity is the main reason LGBTQIA2 youth become homeless.
In addition, Alex Abramovich stated that there are no emergency shelters for LGBTQIA2 youth, and existing shelters offer only binary spaces—for men or women—which do not provide an option for trans youth or those who identify as non-binary.[98] However, some suitable transition houses do exist, including Sprott House in Toronto and Pride Home in Saskatoon. Pride Home is a long-term residence for LGBTQIA2 youth aged 16 to 21 that opened its doors in 2017. This home offers services tailored to non-binary youth. OutSaskatoon, the organization that established and operates Pride Home, told the Committee that the funding needed to operate Pride Home each year is difficult to secure. Federal and provincial housing programs offer funding for capital expenses, but not for wages or operating costs.[99]
Mr. Abramovich recommended that, to help LGBTQIA2 youth who are at risk of becoming homeless, Canada’s homelessness, housing and poverty reduction strategies should focus on these youth. He also recommended that questions on sexual orientation and gender identity be included in all federal health surveys.[100]
Income and Employment
Income and health are closely linked.[101] The ability to hold a stable job and earn a decent living varies from one LGBTQIA2 community to the next. Some transgender youth reportedly have trouble securing a job because they have not necessarily changed their legal name or modified their identification cards, which they need to get a job.[102]
Trans individuals can also face discrimination in the workplace. Tristan Coolman cited the example of a trans woman who participated in the Pflag organization’s activities. She reported being discriminated against wherever she worked in the construction industry. This discrimination took the form of hateful comments or graffiti in bathrooms. Following a period of financial instability, she had to choose between paying her rent and paying for her medication.[103]
Alex Abramovich shared the results of a 2019 study on trans people in Ontario that showed that, of the roughly 2,000 trans people surveyed, 50% live in low-income neighbourhoods, compared with 37% of the general population.[104]
During its meeting with REZO, an organization for gbMSM in Montreal, the Committee learned that certain factors have negative effects on their income, such as the tendency for gay men to be in relationships less often and for less time than heterosexual men. REZO told the Committee that gay men generally earn $8,000 to $12,000 less than heterosexual men.
Food Insecurity
Figure 3 illustrates the rate of food insecurity in Canada by sexual orientation. It reveals that three times more bisexual Canadians report being food insecure than heterosexual individuals. More than one in four bisexual women and at least one in five bisexual men say they experience food insecurity.[105]
Figure 3—Rate of Food Insecurity in Canada, By Sexual Orientation
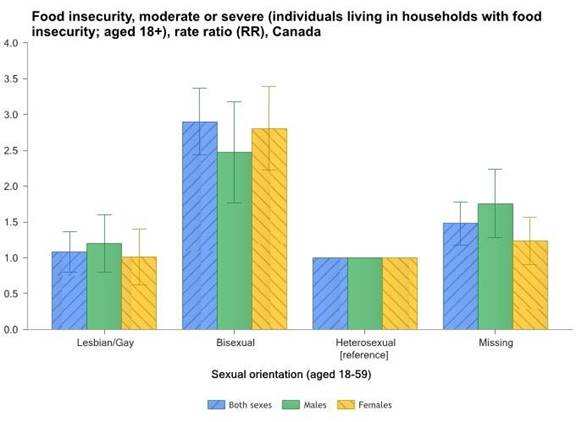
Source: Pan-Canadian Health Inequalities Data Tool, 2017 Edition.
Age
Age affects the health of gender and sexual orientation minorities and their needs. Gerry Croteau of the Gilbert Centre for Social and Support Services told the Committee that, for LGBTQIA2 people who grew up in the 1960s, identifying as LGBTQIA2 was not an option. Part of their lives were lived when being gay could lead to criminal prosecution[106] and was considered a pathology.
LGBTQIA2 people are more likely to live alone than heterosexual people of the same age.[107] For example, aging LGBTQIA2 people are concerned about the possible lack of social support and social isolation if they have health problems.[108]
Witnesses said that older adults have some concerns when moving to a seniors’ residence or using palliative care. During its meeting with the Winnipeg-based Canadian Virtual Hospice, the Committee learned that LGBTQIA2 older adults worry about having to “go back into the closet” if they seek palliative care. They are also concerned that their sexual orientation or gender identity may be disclosed without their consent by their families. They fear receiving lower quality care because of their sexual orientation or gender identity. Similar concerns were raised by witnesses about older adults moving into a seniors’ residence or needing home care.[109]
Indigenous People
Many witnesses said that two-spirit people or Indigenous people who identify as LGBTQIA2 face different levels of discrimination because of their sexual orientation or gender identity, Indigenous origins and sometimes their HIV positive status or whether they have hepatitis C.[110] The Committee learned that two-spirit people may also face discrimination within Indigenous communities.[111]
Access to Health Care
Witnesses gave various examples of barriers that affect access to health care for members of gender and sexual minorities. First, not all LGBTQIA2 people inform their doctors about their sexual orientation or behaviour and gender identity. Jody Jollimore, Executive Director of the Community-Based Research Centre, said that outside Vancouver, in northern British Columbia communities, up to 60% of LGBTQIA2 people do not talk to their health care provider about their sexual orientation.[112] People who do not inform their doctor of their sexual orientation are also less likely to be tested for HIV based on their risk factors.
Several sexual and gender minorities also said that they often need to educate health professionals about their risk factors or health needs.[113] Moreover, health care workers will refuse to treat people belonging to sexual or gender minorities because they do not feel that they are sufficiently trained—which can lengthen the time it takes for these people to access care.[114]
Access to Health Care for Trans People
The Committee was told that access to health care for trans people is particularly difficult.[115] They underuse health services, including emergency services. Between 20% and 30% of trans people who needed emergency services did not go to the hospital and 52% of those who did had a negative experience.[116]
For trans people who want to change their sex, coverage for gender affirming surgeries varies widely from province to province[117] and requires letters of recommendation from a psychiatrist, psychologist or other health professionals. Loretta Fearman, with Pflag Canada, gave an example to illustrate the problem:
When they sought a referral for top surgery, they decided to go to Montreal, since Toronto wait times were one year longer. The medical documentation required for surgery approval was arduous. It resulted in multiple visits to several professionals simply for the purpose of filling out paperwork. The wait for approval was significant. Once approved, only then could Tom go on the wait-list at the Montreal clinic.[118]
In addition to delays, the need to obtain letters of recommendation for gender affirming surgeries may create financial barriers since some health professionals (psychologists, psychotherapists, social workers) work in the private sector. Washington Silk also questioned the fact that a health professional must certify a person’s gender identity when 53% of trans people must educate health professionals about their situation.[119] The Canadian Professional Association for Transgender Health recommends that the informed consent model be used in the offer of health care for trans people.[120]
Witnesses and organizations that submitted briefs also noted that long delays in access to gender affirming surgery increase the risk of depression and suicidal ideation among trans people.[121]
In the context of access to health care, trans people in particular may be asked questions wholly unrelated to the reason for their consultation. Witnesses gave an example of a trans person being refused services for a foot injury because “we don’t treat trans people who take hormones”[122] and a trans woman who did not receive care for a streptococcal infection because she was taking hormones.[123]
Gisèle Bloch, with Toronto Pflag, told the Committee that misgendering—the use of the wrong gender, pronoun or name—has harmful effects on trans people and can prevent them from accessing adequate health care. She said:
…a woman told me about the time she went to a lab for some blood work. She presents feminine, but she hasn't received her new ID yet. When she handed in her requisition and ID to the receptionist, she politely asked if the technician could please use her new female name when she was called. When the technician bellowed out her old male name, she froze. The technician called the name again and she was immobilized. Then the receptionist stood up, pointed to her and said loudly, “That's him.”…she just sat there crying…until she finally found the strength to run out of the lab without getting her blood work done.[124]
Racialized People and Newcomers
“Oftentimes in racialized communities, our queerness is erased; and in queer communities, our racialized identities are not welcome.”[125]
The Committee learned that homosexuality is still stigmatized in some racialized communities and that it is not always better to come out of the closet in this context. Darren Ho, Founder, Our City of Colours, told the Committee that some LGBTQIA2 individuals from minority cultures do not know the word “queer” in their mother tongue because the word does not exist or they have not learned it.[126]
These contexts must be taken into account in access to health care. In this regard, Darren Ho recommended anonymous and confidential sexual health service options for racialized people.[127] He also recommended developing positive messaging and programs on the diversity of sexual orientation and gender identity in languages other than English and French, as well as resources for newcomers and refugees.[128]
REZO told the Committee during its trip to Montreal that resources in Spanish and Arabic need to be developed to reach LGBTQIA2 people in Montreal’s ethnocultural communities. REZO said that every region in Canada has a different reality in terms of ethnocultural make-up and immigration, and that resources for LGBTQIA2 people in different regions should be adapted accordingly.
The Centre for Gender Advocacy told the Committee that trans people face barriers to permanent residence. They might have to consult a psychiatrist to assess how their trans identity will impact their health care needs. According to the Centre for Gender Advocacy, having to consult a psychiatrist has been a long, stressful and costly process for these immigrants. They have to comply or risk seeing their file closed.[129]
Place of Residence
Not all types of care are available in remote or rural areas. In the Atlantic region, Arthur Miller, from Healing our Nations, said that people can be tested for HIV or hepatitis C in their community but have to travel to a major centre for treatment.[130] Some people will not go to their first follow-up appointment in these circumstances. Mr. Miller recommended that community staff bridge the gap with urban specialists and that clients be better informed about the next steps in their treatment.[131]
WAYS TO PROMOTE HEALTH EQUITY FOR LGBTQIA2 COMMUNITIES
Witnesses made a series of recommendations to the Committee on what could be done to improve the health of LGBTQI2 people.
Sex Education
Many witnesses stressed the importance of receiving sex education that includes sexual diversity and gender identity in its curriculum. Calgary-based Centre for Sexuality informed the Committee that they have been offering sex education in Alberta’s schools since 1975. Over 10,000 youth receive their program annually.[132] Sarah Chown, Executive Director, YouthCO HIV and Hep C Society, shared the results of a survey her organization conducted with 600 high school students in 80 communities in British Columbia. The survey found that 84% of young people felt that school was an important place to get sex education. In addition, 45% of them said that the sex education they received did not recognize sexual and gender diversity.[133]
Sarah Chown also told the Committee that the Canadian Guidelines for Sexual Health Education have been revised and will be available in 2019. They include sexual and gender minorities. She recommended that they be implemented.[134]
The Committee also heard that age-appropriate sex education should be offered at a young age. Witnesses noted that children should have a sense early on of the diversity in sexual orientation and gender.[135] Alex Abramovich explained that children are rarely exposed to books and teaching materials presenting LGBTQIA2 communities’ realities.[136]
Family and School Support for Youth
Studies show that LGBTQIA2 youth who have supportive environments that allow them to be themselves thrive.[137] As well, a study in British Columbia found a significant drop in suicidal ideation in British Columbia schools that have implemented a gay-straight alliance.[138] Travis Salway, a postdoctoral fellow at the University of British Columbia, said that these alliances are “live-saving.”[139] The Centre for Sexuality in Calgary noted that when LGBTQIA2 youth do not have support from their family or their schools, it can lead to very negative health outcomes.[140]
Trans and non-binary youth are particularly in need of support. Dustyn Baulkham, with the Kelowna Pride Society, said that Kelowna’s peer support group—the Etcetera Youth Group—is attended mainly by trans and non-binary youth, although the group is open to all LGBTQIA2 youth.[141]
Social Connections
Many witnesses said that LGBTQIA2 communities need safe public places to meet and connect with each other. The Internet and smartphone apps, like Grindr, can facilitate virtual connections, but witnesses said that these cannot replace the benefits of physical meeting places. Many LGBTQIA2 people also grapple with isolation.[142]
Unfortunately, several organizations said that they lack funding, or that funding is irregular. This prevents them from offering some activities.[143] Pflag members said that requests for their services, which are provided by volunteers, often exceed the capacity of Pflag chapters.[144]
Digital Health
Studies have shown that sexual and gender minorities tend to use new technologies and the Internet. For example, the GetCheckedOnline website, which offers testing options for some STBBIs, is widely used by gbMSMin British Columbia.[145] Digital health initiatives could provide an opportunity for the federal government to improve the health of LGBTQIA2 people in Canada. Witnesses said that the Canada Health Infoway could develop digital health initiatives for sexual health and that sexual and gender minorities are priorities among Infoway’s work.[146]
Legal Amendments
Non-disclosure HIV Status
To reduce stigma, witnesses and organizations that submitted briefs recommended that the federal government end the criminalization of non-disclosure of HIV status.[147] The Committee heard that HIV treatment is effective in preventing HIV transmission. Dr. Moore noted in his testimony that those “who are receiving treatment HIV treatment and have achieved virologic suppression can now be assured that they will have near-normal life expectancy; equally important, they will not transmit HIV to their sexual partners.”[148]
Surgery on Intersex Children
Witnesses and briefs to the Committee recommended that the section of the Criminal Code that currently allows for surgery on intersex children be reviewed. Egale Canada recommended that a broad consultation with intersex people on subsection 268(3) be held as a first step towards reforming this subsection.[149] Other organizations that submitted briefs were also in favour of revising the content of subsection 268(3) to postpone genital surgeries that aim to normalize the appearance of genitals until the child can consent to such surgery.[150]
Health Provider Training
Several witnesses highlighted the need to improve health provider training at all levels—including among administrative staff, care attendants, nurses, physicians, psychologists and social workers—to include gender diversity and sexual orientation. Andrea Daley, Associate Professor, Renison University College, said that it is important to provide repeated training to health care workers because the goal is not simply acquiring knowledge but changing attitudes towards LGBTQIA2 people.[151] The training should be designed so as not to reproduce stereotypes about LGBTQIA2 people by focusing only on sexuality or mental health issues[152] and should include a component on how to interact with trans people.[153]
CONCLUSION
In this study, witnesses highlighted the importance of introducing measures to prevent and address the health inequities experienced by LGBTQIA2 communities, which overall have poorer physical, mental and sexual health than their heterosexual counterparts. The Committee notes that the lack of acceptance of sexual and gender diversity in Canadian society is an underlying factor in how LGBTQIA2 people are treated and has a major impact on their health.
While the rights of LGBTQIA2 people have greatly improved in recent decades, witnesses said that social equality has not yet been achieved. The Committee notes that each subgroup within LGBTQIA2 communities has specific health vulnerabilities and that an intersectional analysis is needed to identify the most vulnerable people within these communities.
The Committee would like to acknowledge the dedication of all witnesses and organizations to the health of LGBTQIA2 people, as well as the quality of their contribution to the study on the health of LGBTQIA2 communities in Canada. The Committee is also grateful to the witnesses who shared their personal stories or lent their voices to share other stories that will help readers better understand the reality of LGBTQIA2 people in Canada.
The Committee recognizes that the people who know how to improve the health of LGBTQIA2 communities are those who are part of them. They should be involved in the development of policies, programs and decisions affecting their health. The Committee therefore makes the following recommendations which, if implemented, would contribute to improving the health of LGBTQIA2 communities in Canada:
Awareness campaign, education and training
Recommendation 1
That the Government of Canada develop and implement a national awareness campaign on sexual and gender diversity that reflects an intersectional analysis in order to address the stigma and discrimination faced by LGBTQIA2 communities in Canada.
Recommendation 2
That the Government of Canada develop information tools on sexual and gender diversity in both official languages and other appropriate languages as requested.
Recommendation 3
That the Government of Canada ensure that the Public Health Agency of Canada promptly completes the revision of the Canadian Guidelines for Sexual Health Education; that the revised version include the diversity of sexual orientations and gender identities in all areas; and that the updated guidelines are made available across Canada.
Recommendation 4
That the Government of Canada, through Health Canada, work with the provinces and territories to encourage the provision of age-appropriate education on sexual orientation and gender identity to children and youth of all age groups as well as parents and caregivers.
Recommendation 5
That the Government of Canada work with the provinces, territories and provincial health professional and regulatory bodies to establish a working group to identify ways to promote training and education of health care professionals about the health needs of sexual and gender minorities.
Consultation
Recommendation 6
That the Government of Canada, as part of its efforts to modernize its sex and gender information practices, consult with trans and non-binary individuals to establish best practices for collecting gender information and best identification options for non-binary people.
Data collection
Recommendation 7
That the Government of Canada, through Statistics Canada, consult with LGBTQIA2 organizations, researchers and LGBTQIA2 individuals to help the agency develop and include questions on sexual behaviour and sexual attraction in its surveys.
Recommendation 8
That the Government of Canada, through Statistics Canada, promote the oversampling of LGBTQIA2 populations in its surveys in order to produce samples of sufficient size for intersectional analyses.
Recommendation 9
That the Government of Canada, through Statistics Canada, include questions on sex at birth, gender identity and sexual orientation in all its surveys regardless of respondent age and on a priority basis in surveys on health, housing, income, homelessness and the use of alcohol, tobacco and other substances.
Research funding
Recommendation 10
That the Government of Canada, through the Canadian Institutes of Health Research, include sexual orientation and gender identity in the mandate of the Institute of Gender and Health to ensure sustained funding for research on the health of LGBTQIA2 communities.
Program funding
Recommendation 11
That the Government of Canada, through Health Canada and the Public Health Agency of Canada, establish a grants and contributions program focussing on the health of LGBTQIA2 communities to ensure that LGBTQIA2 organizations have their own funding stream to improve the health of these communities.
Target LGBTQIA2 communities within existing public policies and programs
Recommendation 12
That the Government of Canada establish an advisory committee on sexual and gender minorities to support departments in their efforts to implement LGBTQIA2 community-specific measures as part of the National Housing Strategy, Canada’s Homelessness Strategy, Canada’s Poverty Reduction Strategy, Canada’s Tobacco Strategy and the Canadian Drugs and Substances Strategy.
Recommendation 13
That the Government of Canada’s funding of shelter spaces consider the needs of trans and non-binary individuals for non-gendered options.
Health of trans people
Recommendation 14
That the Government of Canada, in collaboration with the provinces and territories, provide coverage for the cost of hormones required for the health of trans people as part of the development of a national pharmacare program, as recommended by the Standing Committee on Health in its report entitled Pharmacare Now: Prescription Medicine Coverage for all Canadians.
Recommendation 15
That the Government of Canada work with the provinces and territories to ensure uniform coverage across Canada for gender affirming surgeries and other medical care for trans people.
Sexually transmitted and blood-borne infections
Recommendation 16
That the Government of Canada, through Health Canada, expedite the licensing process for home test kits and self-screening tools for human immunodeficiency virus and other sexually transmitted and blood-borne infections.
Recommendation 17
That the Government of Canada, through the Public Health Agency of Canada and the National Advisory Committee on Immunization, encourage the provinces and territories to modify the recommended vaccination schedule for the human papillomavirus vaccine to achieve universal coverage, particularly for young men and adult men who have sex with men.
Recommendation 18
That the Government of Canada, in collaboration with the provinces and territories, provide prescription drug coverage of antiretroviral drugs used in the treatment and prevention of HIV/AIDS at little or no cost to Canadians as part of the development of a national pharmacare program, as recommended by the House of Commons Standing Committee on Health in its report entitled Pharmacare Now: Prescription Medicine Coverage For All Canadians.
Recommendation 19
That the Government of Canada, through the Public Health Agency of Canada, update the Canadian Guidelines on Sexually Transmitted Infections and national resources to reflect the diversity of gender identities and sexual orientations and integrate the links between mental health and sexual health.
Recommendation 20
That the Government of Canada increase total funding for the Federal Initiative to Address HIV/AIDS in Canada to $100 million annually, as recommended in the 2003 report of the Standing Committee on Health entitled Strengthening the Canadian Strategy on HIV/AIDS.
Conversion therapy
Recommendation 21
That the Government of Canada work with the provinces and territories to eliminate the practice of conversion therapy in Canada and consider making further modifications to the Criminal Code.
Intersex people
Recommendation 22
That the Government of Canada hold consultations with intersex people and stakeholders on subsection 268(3) of the Criminal Code, which allows for surgeries on intersex people, and consider the postponement of genital normalizing surgeries on children until the child can meaningfully participate in the decision, except where there is immediate risk to the child's health and medical treatment cannot be delayed.
Blood, organ and tissue donation
Recommendation 23
That the Government of Canada end all discriminatory practices related to blood, organ and tissue donation for men who have sex with men and trans people and adopt donor screening policies that are evidence-based, gender neutral, and behaviour-based.
[1] House of Commons Standing Committee on Health [HESA], Minutes of Proceedings, 1st Session, 42nd Parliament, 16 April 2018.
[2] A gender and sexual diversity glossary is provided in Appendix A.
[3] The witnesses used variations of this abbreviation such as LGBT, LGBTQI2S, LGBTQI2S+ and 2SLGBTQ.
[4] HESA, Evidence, 1st Session, 42nd Parliament, 30 April 2019, 1600 (Joël Xavier, Administrator, Conseil québécois LGBT).
[5] HESA, Evidence, 28 February 2019, 1645 (Lori Ross, Associate Professor, Dalla Lana School of Public Health, University of Toronto).
[6] HESA, Evidence, 9 April 2019, 1540 (Alex Abramovich, Independent Scientist, Centre for Addiction and Mental Health, Institute for Mental Health Policy Research, As an individual).
[7] HESA, Evidence, 7 May 2019, 1530 (Jack Woodman, President, Canadian Professional Association for Transgender Health).
[8] Ibid., 1550 (Quinn Bennett, Provincial Lead, Peer and Community Support Networks, Trans Care BC, Provincial Health Services Authority).
[9] Conseil québécois LGBT, Brief Submitted to the Standing Committee on Health for Its Study on the Health of LGBTQ2 Communities, April 2019; Canadian Bar Association, LGBTQ2 Health in Canada, May 2019.
[10] Albert McLeod, “Two-Spirit Resurgence in the 21st Century,” PowerPoint presentation to HESA during its trip to Winnipeg, 2 April 2019.
[11] HESA, Evidence, 7 May 2019, 1600 (Sarah Chown, Executive Director, YouthCO HIV and Hep C Society).
[12] HESA, Evidence, 9 May 2019, 1640 (Jeff Chalifoux, Coordinator, Harm Reduction Program, Edmonton Men’s Health Collective); HESA, Evidence, 7 May 2019, (Lorraine Grieves, Provincial Program Director, Trans Care BC, Provincial Health Authority); Ontario Federation of Indigenous Friendship Centres, Submission to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019.
[13] Statistics Canada, Brief to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019.
[15] Ibid.
[18] Statistics Canada, Brief to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019.
[19] HESA, Evidence, 9 April 2019, 1550 (Greg Oudman, Executive Director, Health Initiative for Men).
[20] HESA, Evidence, 28 February 2019, 1545 (Ross); Statistics Canada, Brief to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019.
[21] Toronto Bisexual Network, Brief on Bisexual Mental Health, May 2019; Statistics Canada, Brief to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019.
[23] Ibid.
[24] Jane Pyne et al., Submission to the Federal Standing Committee on LGBTQ+ Health to Consider Taking Action regarding the Harms of Conversion Therapy, May 2019; Generous Space Ministries, Preventing and addressing the harm caused by sexual orientation and gender identity change efforts, May 2019; Travis Salway et al, Protecting Canadian sexual and gender minorities from harmful sexual orientation and gender identity change efforts, May 2019; Florence Ashley, Submission to the House of Commons Standing Committee on Health for the Study on LGBTQ2 Health in Canada on the Matter of Conversion Therapy, May 2019.
[25] Sexual Orientation and Gender Identity Protection Act, ch. 28 of the Acts of 2018.
[26] Health Insurance Act, R.S.O. 1990, c. H.6; Regulated Health Professions Act, 1991, S.O. 1991, c. 18.
[27] HESA, Evidence, 9 April 2019, 1535 (Travis Salway, Post-doctoral Research Fellow, School of Population and Public Health, University of British Columbia, As an individual).
[28] Ibid.
[29] Generous Space Ministries, Preventing and Addressing the Harm Caused by Sexual Orientation and Gender Identity Change Efforts, May 2019.
[31] Ibid.; Generous Space Ministries, Preventing and Addressing the Harm Caused by Sexual Orientation and Gender Identity Change Efforts, May 2019; Florence Ashley, Submission to the House of Commons Standing Committee on Health for the Study on LGBTQ2 Health in Canada on the Matter of Conversion Therapy, May 2019.
[33] Statistics Canada, Brief to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019.
[34] HESA, Evidence, 28 February 2019, 1535 (MacFarlane); Rainbow Health Ontario, LGBTQ2 Health in Canada: Study Brief for the Standing Committee on Health, May 2019.
[35] Canadian Cancer Society, Human papillomavirus (HPV) infection.
[36] HESA, Evidence, 2 May 2019, 1615 (Dr. Tinus Wasserfall, Family Doctor, Spectrum Health, As an individual).
[37] HESA, Evidence, 11 April 2019, 1530 (Dr. Mark Gilbert, Medical Director, Clinical Prevention Services, BC Centre for Disease Control).
[39] HESA, Evidence, 11 April 2019, 1540 (Dr. David Moore, Research Scientist, Epidemiology and Population Health Program, British Colombia Centre for Excellence in HIV/AIDS).
[40] Ibid.
[42] Ibid.
[43] HESA meeting with Head and Hands, Montreal, 1 April 2019.
[45] Ibid.
[46] Five federal drug coverage plans include: the Non-Insured Health Benefits Program for Registered First Nations persons and Inuit recognized by an Inuit land claim organization; Interim Federal Health Program for select refugee protection claimants; Veterans Affairs Prescription Drug Program for veterans and members of the Royal Canadian Mounted Police; Correctional Service Canada for federal inmates and Canadian Forces Health Services. For further details please see: HESA, “Pharmacare Now: Prescription Medicine Coverage For All Canadians,” 1st Session, 42nd Parliament, April 2018.
[47] For further details, please see: Deborah Yoong et al, “Public Prescription drug plan coverage for antiretrovirals and the potential cost to people living with HIV in Canada: a descriptive study.” In Canadian Medical Association Journal, Vol. 6, No. 4, 27 November 2018.
[48] For further details, please see: HESA, “Pharmacare Now: Prescription Medicine Coverage for All Canadians: Appendix A,” 1st Session, 42nd Parliament, April 2018.
[49] Ibid.
[50] HESA, Evidence, 11 April 2019, 1535 (Gerry Croteau, Executive Director, Gilbert Centre for Social and Support Services).
[51] Gary Lacasse, Executive Director, Canada, AIDS Society, “Written Response to Questions” submitted to HESA, 15 April 2019.
[53] Ibid., 1535 (Moore).
[54] Ibid., 1610 (Moore).
[55] Health Canada and the Public Health Agency of Canada, Written Brief for HESA Study on LGBTQ2 Health in Canada, May 2019.
[56] Joseph Erban and Dr. Michael Dworkind, Tobacco Use and the LGBTQI2 and HIV/AIDS Communities in Canada, May 2019.
[57] Government of Canada, Canadian Tobacco Use Monitoring Survey (CTUMS) 2012.
[58] Government of Canada, Canada’s Tobacco Strategy.
[59] Kieffer G. Card et al., Improving Substance Use Related Policies for Gay, Bisexual, and Queer Men, May 2019.
[60] HESA meeting with REZO, Montreal, 1 April 2019.
[63] Statistics Canada, Brief to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019; HESA, Evidence, 28 February 2019, 1545 (Ross).
[64] Statistics Canada, Brief to the Standing Committee on Health: LGBTQ2 Health in Canada, May 2019.
[65] Ibid.
[66] Lori Ross et al., Enhancing Our Evidence Base to Characterize and Monitor LGBTQ2 Health in Canada, April 2019.
[67] Ibid.
[68] HESA, Evidence, 30 April 2019, 1540 (Gabriel Girard, Researcher, Sociologist, Centre de recherche de Montréal sur les inégalités sociales et les discriminations).
[69] Lori Ross et al., Enhancing Our Evidence Base to Characterize and Monitor LGBTQ2 Health in Canada, April 2019.
[70] The diagnosis of homosexuality was listed in the Diagnostic and Statistical Manual (DSM) of psychiatric disorders until 1973.
[72] Ibid., 1705 (Rachel Loewen Walker, Executive Director, OUTSaskatoon); HESA, Evidence, 2 May 2019, 1630 (Crystal Fach, Co‑Founder, Diversity ED), DisAbled Women’s Network of Canada, Health Issues for LGBTQ2 People with Disabilities, May 2019; Quebec Lesbian Network, Specific Challenges Related to the Physical, Mental and Sexual Health of LGBTQ+ Women, April 2019.
[74] Ibid.
[75] Ibid.
[76] HESA, Evidence, 9 April 2019, 1625 (Tristan Coolman, President, Pflag York Region); HESA meeting with Mike Morrison, Calgary, 4 April 2019.
[80] HESA, Evidence, 7 May 2019, 1540 (Washington Silk, Program Coordinator and Registered Social Worker, Psychotherapist, OK2BME, KW Counselling Services).
[83] HESA, Evidence, 9 May 2019, 1540 (Bill Ryan, Adjunct Professor, School of Social Work, McGill University, As an individual).
[84] HESA, Evidence, 11 April 2019, 1550 (Lacasse); HESA, Evidence, 30 April 2019, 1555 (Jody Jollimore, Executive Director, Community-Based Research Centre); COCQ-SIDA, Brief for the Study on LGBTQ2 Health in Canada, May 2019.
[85] Government of Canada, Fact Sheet – HIV Non-Disclosure and the Criminal Law, December 2017.
[86] Ibid.
[87] Government of Canada, “Attorney General of Canada to issue Directive Regarding Prosecutions of HIV Non-Disclosure Cases,” News release, 1 December 2018.
[88] House of Common Standing Committee on Justice and Human Rights, 42nd Parliament, 1st Session, Minutes of Proceedings, 8 June 2017.
[89] HESA, Evidence, 28 February 2019, 1555 (Richard Matern, Director of Research and Policy, Egale Canada).
[92] Queer Ontario, LGBTQ2 Health in Canada, May 2019.
[93] According to Health Canada, the determinants of health include a wide range of personal, social, economic and environmental factors that influence individual and population health.
[95] Ibid., 1700 (Jollimore).
[96] Health Canada and the Public Health Agency of Canada, Written Brief for HESA Study on LGBTQ2 Health in Canada, May 2019.
[97] HESA, Evidence, 9 April 2019, 1540 (Abramovich); HESA, Evidence, 30 April 2019, 1620 (Martha Smith‑Norris, Board Chair, OUTSaskatoon).
[101] Ibid.
[102] Ibid., 1645 (Abramovich).
[103] Ibid., 1600 (Coolman).
[104] Ibid., 1545 (Abramovich).
[105] Health Canada and the Public Health Agency of Canada, Written Brief for HESA Study on LGBTQ2 Health in Canada, May 2019.
[107] Kimberley Wilson and Arne Stinchcombe, Policy Legacies and Forgotten Histories: Health Impacts on LGBTQ2 Older Adults, May 2019.
[108] Ibid.
[109] HESA, Evidence, 28 February 2019, 1540 (MacFarlane); HESA, Evidence, 11 April 2019, 1615 (Lacasse, Croteau).
[110] HESA meeting with Albert McLeod, Two-Spirited People of Manitoba, Winnipeg, 2 April 2019; HESA, Evidence, 9 May 2019, 1600 (Miller).
[113] HESA, Evidence, 9 May 2019, 1535 (Andrea Daley, Associate Professor, School of Social Work, Renison University College, University of Waterloo, As an individual).
[116] HESA, Evidence, 9 May 2019, 1530 (Daley); Evidence, 30 April 2019, 1600 (Xavier); Canadian Professional Association for Transgender Health, Brief to the Standing Committee on Health, May 2019.
[117] Appendix B contains information on provincial coverage of various surgeries and gender affirming procedures.
[118] HESA, Evidence, 2 May 2019, 1605 (Loretta Fearman, Chapter Facilitator, Barrie-Simcoe County, Pflag Canada).
[119] HESA, Evidence, 7 May 2019, 1540 (Silk); The 519, Brief for the Standing Committee on Health, May 2019.
[120] Canadian Professional Association for Transgender Health, Brief to the Standing Committee on Health, May 2019.
[121] Emery Potter and Kate Greenaway, Brief Submitted to the Standing Committee on LGBTQ2 Health in Canada, May 2019.
[123] HESA meeting with the Centre for Sexuality, Calgary, 4 April 2019.
[126] Ibid., 1615.
[127] Ibid., 1610.
[128] Ibid., 1615.
[129] Centre for Gender Advocacy, Brief for the Standing Committee on Health, May 2019.
[130] HESA, Evidence, 9 May 2019, 1605 (Arthur Miller, Community Health Educator, Healing Our Nations).
[131] Ibid.
[132] HESA meeting, Centre for Sexuality, Calgary, 4 April 2019.
[134] Ibid., 1605.
[136] Ibid., (Abramovich).
[137] Stigma and Resilience Among Vulnerable Youth Centre, Brief Submitted to the Standing Committee on Health for the Committee's Study of LGBTQ2S Health in Canada, May 2019.
[138] Ibid.
[140] HESA meeting, Centre for Sexuality, Calgary, 4 April 2019.
[142] HESA meeting with Head & Hands, Montreal,1 April 2019; HESA, Evidence, 2 May 2019, 1555 (Baulkham).
[146] Ibid.
[147] Canadian Bar Association, Health of the LGBTQ2 Community in Canada, May 2019.
[150] Canadian Bar Association, Health of the LGBTQ2 Community in Canada, May 2019.
[152] Ibid., 1630.